The gut microbiota can impact the effectiveness of anti amoeba medications. It is thought to alter the drug’s metabolism and bioavailability and the host’s immune response to E. histolytica infection.
Introduction
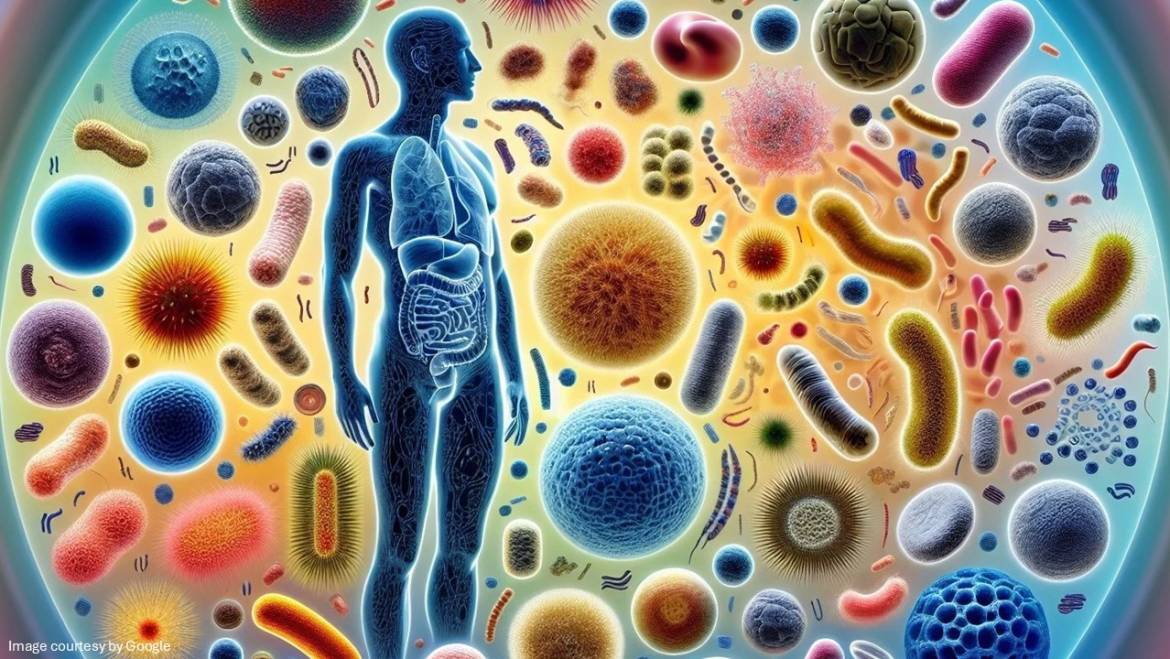
What is gut microbiota? Gut microbiota is defined as a group of microorganisms that are deposited throughout the entire gastrointestinal tract (GI) and are present in a higher proportion than the cells of the human body. The human gut microbiome (the community of microorganisms) comprises up to 100 trillion microbes. These unique populations of viruses, bacteria, and fungi living in the gastrointestinal tract are important for the innate maintenance of health. The microbiota regulates a wide range of vital functions for human health.
About Amebiasis
The protozoan parasite Entamoeba histolytica causes amebiasis. The main symptoms are a liver abscess and inflammation of the large intestine. The condition is caused by the consumption of food contaminated with cysts, the parasite’s infective form. It occurs relatively infrequently; however, in many cases, symptoms are not observable. Host and parasite factors likely cause infection with the parasite. However these factors can’t completely explain the wide variation presentation in patients. Therefore, an environmental factor causes the progression of E histolytica infection. The infection with E. histolytica occurs after ingestion of foods containing E histolytica cysts or after ingestion of faecally contaminated water. Moreover, some strains of E.histolytica are less sensitive to Metronidazole, contributing to the emergence of metronidazole-resistant strains. No vaccination is available yet against amoebiasis; the medicine of choice for treating amoebiasis is Metronidazole.
Large intestine and its associated microbiota
As mentioned above, the human intestine carries more than 100 trillion bacteria, which represent 500 to 1000 species. These bacteria play an important role in producing vitamins and other metabolites that are important to the host. The gut microbiota has a close association with human health. Once there is any disturbance in the intestinal flora, a series of intestinal disorders, such as colorectal cancer and inflammatory bowel syndrome, may occur. The establishment of gut microbiota starts even before birth to achieve a stable level by 2 to 5 years of age. Numerous factors are responsible for affecting the composition of gut microbiota following birth, which include the type of delivery, intake of breastmilk vs formula, hygiene status, and antibiotic treatment. In adults, the gut microbiota is generally stable, but it can change with diet and age. In older adults, there are fewer Bifidobacteria, Bacteroides, and Enterobacteriaceae in their gut and more Clostridium species than in younger adults.
Change in the large intestine microbiota following infection with E.histolytica
Over the last few years, it has become clear that E histolytica’s ability to produce disease is directly associated with the parasite’s interaction with the gut microbiota.
The gut flora of patients suffering from amebiasis shows a significant reduction in the population of Clostridium, Bacteroides, Campylobacter, and Lactobacillus and an increase in Bifidobacterium. At the same time, there is no change in Ruminococcus as compared to healthy patients.
Clostridiales Ruminococcaceae, or Prevotella copri, were central for the identification of patients infected with inflammatory bowel syndrome. It is still unknown how a specific gut microbiota relates to patients infected with Entamoeba.
Drug bioavailability and metabolism
The gut microbiota may affect the bioavailability of anti-amoebic medicines through microbial enzyme activity, disrupting drug transport, or modifying gastrointestinal properties. It affects how much medicine is absorbed and how it travels through the body. It metabolizes drugs, reducing their bioavailability or sometimes converting them into inactive or even toxic metabolites. Also, the gut microbiota can affect enterohepatic recirculation, where medicines are metabolized in the liver and then get back to the gut through bile, affecting their overall exposure.
Affecting the immune response
The gut microbiota is crucial for maintaining the immune system function, including the response to E. histolytica. An imbalance in the gut microbiota (dysbiosis), which can be caused by infection or antibiotic use, can interfere with these processes and affect the severity of the amoebic infections.
Probiotics
Several research studies demonstrated that probiotics may offer an alternative strategy for treating and preventing amoebiasis. These could be effective at restoring healthy gut bacteria, improving the effectiveness of conventional treatments, or preventing infection.
Impact on anti-amoebic medicines
What are anti amebics? These medications are useful in treating infections caused by the protozoan Entamoeba histolytica.
The response to and metabolism of medicines entering the human body vary widely across individuals. One reason is that such interpersonal differences may be associated with gut microbes. On one hand, medicines entering the body may affect the composition of the gut microbiome.
-
- Metronidazole: Metronidazole is considered the first-line treatment for amoebiasis and is known to have some side effects. The microbiota metabolizes Metronidazole, reducing its effectiveness.
- Tinidazole: Tinidazole is considered more effective than Metronidazole; its interaction with the gut microbiota is also a factor.
- Other anti amebics: The effect of microbiota on other anti-amoebic agents is also being investigated, highlighting the potential for personalized medicine based on individual gut microbiota.
Verdict!
The gut microbiota is not just a silent community of microbes in the gut that actively interacts with medicines and the body’s immune response but also impacts the efficacy of amoebiasis treatment and affects the severity of the disease. Understanding these interactions is important for optimizing medicinal therapy and potentially developing personalized drug approaches according to the individual’s gut microbiota profiles.