Stress is considered one of the major contributors to migraine and tension-type headache in adolescents. This article investigates the connection between migraine and stress and evaluates its implications for managing migraine.
Understanding migraine
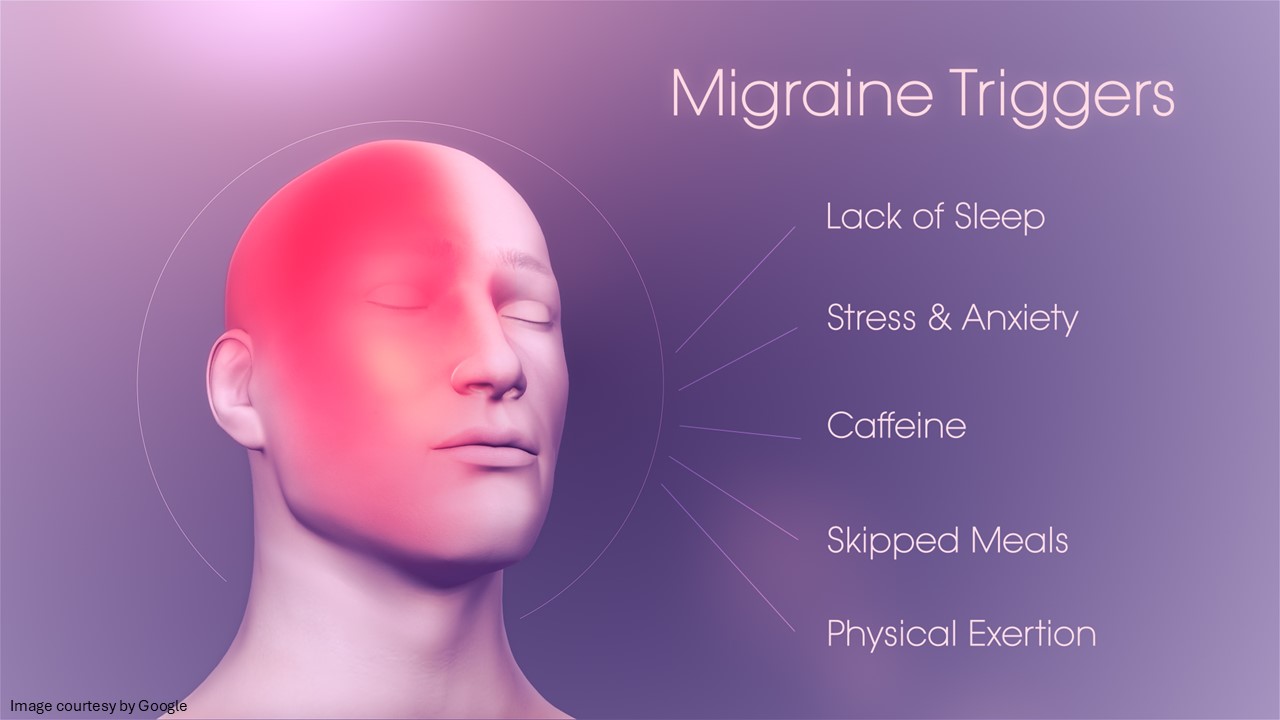
Migraine is a neurological disorder that contributes to a wide range of symptoms, including pulsing, throbbing pain on one or both sides of the head. Migraine pain is most often felt around the temples or behind one eye. One may experience this pain anywhere for hours to days. Migraines are often accompanied by other symptoms such as nausea, vomiting, and light sensitivity. Migraines are not like headaches. The cause/s behind them is not well understood. But there are known triggers, which include stress, among others. One of the possible triggers for migraine attacks is identified as the relaxation following a period of high stress. Meaning, many people experience stress-induced migraine after stress ends, such as on weekends and during vacations. Once the stress calms down, the body struggles to rebalance hormone levels and nervous system activity. This sudden shift can contribute to migraine attack, even though you are finally at a resting state.
Migraine vs stress headache: Tension headaches are steady, dull, and feel like a tight band, whereas migraines are throbbing, severe, and often accompanied by nausea, vomiting, and extreme light- and sound-sensitivity.
Migraines are a neurological condition that affects millions of people worldwide, including an estimated 45 million Americans. It is a complex condition and considered a continuous process in terms of the peri-headache changes in episodic migraine, but also the progression to high-frequency and chronic headache. Thus, it affects the brain system in numerous ways. These include physiological and behavioural responses, such as cardiovascular and immunological changes, as well as pain.
The response to a migraine attack and associated pain, affective changes, stress hormones, nausea/vomiting, etc., is mediated through increased activity of mediators that are present more than normal adaptive processes (involve the brain’s attempt to maintain stability against repeated triggers). Over time, these stressors could alter brain state, including increased cortical excitability, changes in behaviour, and alterations in brain morphology. Such stressors are typically repeated periodically in both cases of chronic daily headache and episodic migraine. This ultimately causes the brain to respond abnormally to environmental conditions, whether it is psychological or physiological. Understanding the pathophysiological changes in brain structure as well as function during a migraine episode may help to get an improved understanding of the neurological condition that frequently affects individuals for a significant portion of their lives.
Stress and migraine
Can stress cause migraines? Though the exact causes of migraine are still not known, researchers believe that it may occur due to changes in the level of certain chemicals in the brain, such as serotonin, which helps regulate pain. In research studies, it has been found that stress is a trigger for migraine episodes in most people. Apart from stress itself, some people believe relaxation after high levels of stress may trigger a migraine. If stress triggers migraines for you, finding ways to reduce your stress is worth the effort. According to the American Migraine Foundation, reducing stress can reduce your symptoms.
Stress is considered a trigger for migraine attacks in most individuals. Excessively high levels of stress have been found in migraine patients, particularly in those who have chronic daily migraine. Both internal stressors (e.g., hormones) and physical (light) or psychological stressors) increase the load on the disease. Physical (abuse, particularly in childhood) and emotional trauma, or social stress, are included in psychological stress. Some women experience menstrual migraine, or their migraines, especially around the menstrual period, could be more intense or even last longer. In addition, stress–induced migraine is simultaneously present with numerous brain diseases that are related to stress and other contributing factors (such as anxiety and depression). Even in children, stress plays an important role.
Children with migraine have higher diastolic pressure, increased pulse rate, and higher low-frequency after a five-minute recovery from an emotional stressor. Once the frequency of these stressors increases, the allostatic response (the body’s active adaptive process of maintaining stability by adjusting physiological points in response to environmental, psychological, or physical stressors) that maintains a stable state for the brain becomes overused. This results in wear and tear on the brain, medically termed allostatic load, which may alter brain networks both functionally and structurally. This causes the brain to respond abnormally to stressors, leading to an altered state and further allostatic load. Normally, the brain responds adaptively to stressors, ranging from psychological to genetic, to maintain a stable brain state. In migraine, the effect of stressors becomes maladaptive (meaning not adjusting to the environment or situation), and this maladaptive response triggers brain changes that shift the brain to a new state.
Effects of repeated migraines on the brain
There is multiple evidence that suggests that migraine brain is different compared to the normal brain. A migraine patient’s brain is hyperexcitable between attacks. During the attack, the brain’s response to certain stimuli is abnormal. For many patients, smells, light, or noise can worsen migraine pain while they are experiencing a migraine episode. Hyperexcitability of the brain can result from reduced levels of GABA or glutamate (neurotransmitters) in the cortical region.
Relationship between stress and migraines: Studies have demonstrated an association of uncertain causality between high stress loads from stressful life events, daily hassles, or other sources and the incidence of new-onset migraine. Major stressful life events contribute to the transformation from episodic to chronic migraine. There is some evidence for changes in stress levels as a risk factor for migraine attacks.
Takeaway!
The exact association between stress and migraine attacks or the increased burden of migraine is still not understood. Several individuals benefit from stress-oriented therapies, and such therapies should be introduced in combination with conventional treatment to treat stress-induced migraine. Understanding the relationship between stress and migraine means that effective treatment options are likely to improve.



