Have you ever thought that diabetes and eye health may be interconnected? Well, having diabetes mellitus type 1 or 2 may make you more likely to develop eye problems that can affect your vision.
This article examines the relationship between diabetes and eye conditions, the impact of diabetes on the eyes, and the most common eye diseases associated with diabetes, as well as the importance of diabetes and eye care management.
Diabetes mellitus is defined as a chronic metabolic condition that affects millions of people worldwide, altering the body’s ability to process glucose, or sugar, found in food. It generally develops when your body either doesn’t produce an adequate amount of insulin (the hormone responsible for regulating blood sugar levels) or is unable to use the insulin it produces. While most people are aware of the impact of diabetes on blood glucose levels, kidney, and heart health, very few know about the effect of diabetes on eye health. In fact, diabetic retinopathy is the major cause of blindness in working-age adults. The diabetes associated eye condition can affect both eyes. It usually develops when high blood sugar damages blood vessels in a certain part of the eye called the retina. Damaged blood vessels can swell and leak, contributing to blurry vision. The condition can affect both eyes. Understanding the link between diabetes and eye damage is essential not only for those who are suffering from diabetes but also for the caregivers and anyone at risk for developing the metabolic disorder.
Effect of diabetes on the eye
Diabetes affects your delicate eyes when glucose levels are excessively high. In the short term, you are not likely to experience diabetes and the eyes symptoms such as vision problems or loss of eyesight. In some cases, when people switch to a diabetes care plan or medication, they may experience blurry vision for a few days or weeks. Elevated blood sugar can interfere with fluid levels in the body, contributing to swelling in the tissues (that help you concentrate) of your eyes, and causing blurred vision. However, the type of blurry vision is temporary and resolves when you achieve normal blood sugar goals. High blood sugar that remains high over time can contribute to damage to the tiny blood vessels in the back of your eyes. This damage can start during prediabetes when the blood sugar is excessively high but not so high that you are diagnosed with diabetes. Abnormal or damaged blood vessels may swell and may leak fluid. New, weak blood vessels begin growing. These blood vessels start to bleed into the middle part of the eye, resulting in scarring or causing excessively high pressure inside the eye, which can be life-threatening. Therefore, managing your diabetes by controlling blood sugar levels is crucial to preventing the progression of diabetes and eye damage
Common eye conditions linked to diabetes
Most serious diabetic eye disease starts with blood vessel issues. Here are diabetes and eye conditions that can affect your vision:
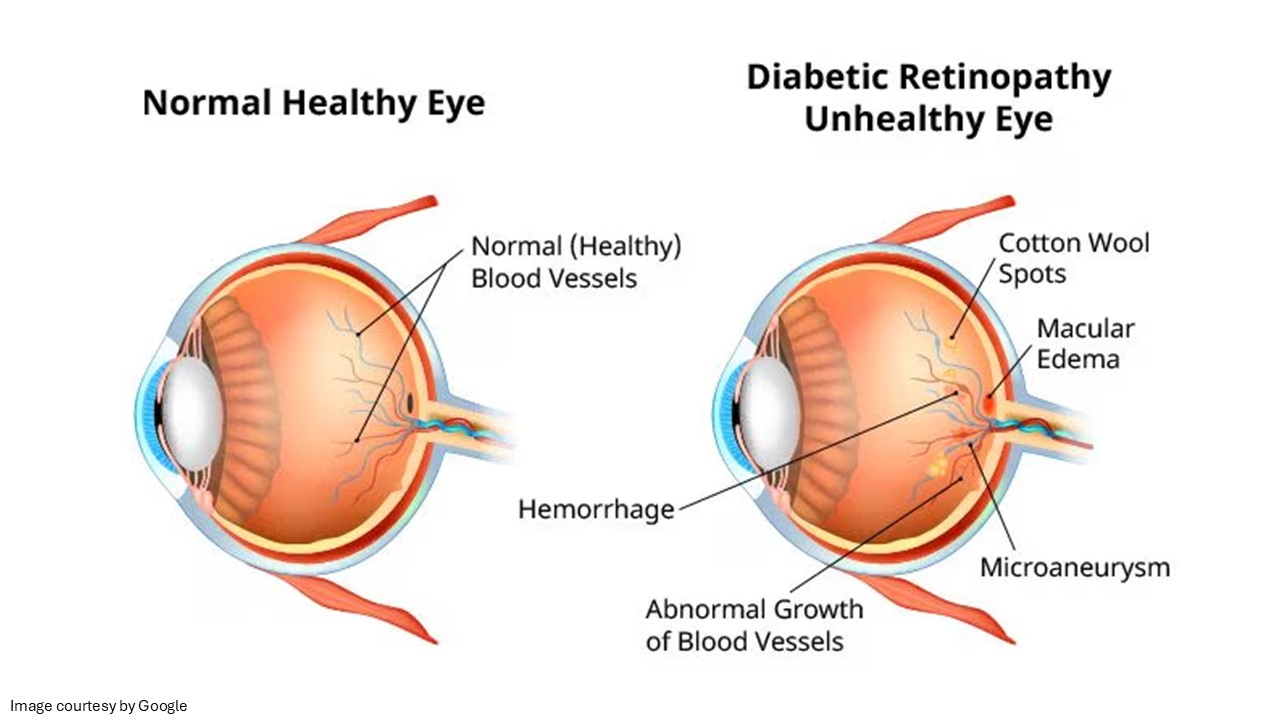
Diabetic retinopathy – One of the most common diabetes-related complications is diabetic retinopathy. The condition occurs when high blood glucose levels persist for an extended period, damaging the tiny blood vessels in the retina. In the back of the eye, the retina is the light-sensitive layer of tissue. At the early stages of diabetic retinopathy, blood vessels can weaken, leading to damage to the retina. If the condition exacerbates (advanced stage), some blood vessels close off, and as a result, new blood vessels grow on the retinal surface. These unusual blood vessels can lead to significant vision problems.
Diabetic macular oedema (DME) – The macula is the part of your retina that helps you with reading, driving, and seeing faces. High sugar levels can cause the macula to swell, a condition referred to as macular oedema. In the long term, diabetes can destroy the sharp vision in the macula region, resulting in partial vision loss or blindness. Macular oedema is an eye condition that typically develops in individuals who already show other symptoms of diabetic retinopathy.
Glaucoma – Glaucoma is an eye disorder that may cause damage to the optic nerve (a bundle of nerve fibres that joins the eye to the brain). The chronic metabolic disorder almost doubles the chances of having glaucoma, which can contribute to blindness if left untreated. Diabetes and eye symptoms depend on the type of glaucoma you have.
Cataracts – You have lenses that are clear enough to provide sharp vision, but with age, they become cloudy. Diabetes patients are more likely to develop cloudy lenses, a condition often referred to as cataracts. Diabetes patients can get cataracts at an early stage compared to people without diabetes. According to clinical findings, high sugar levels cause deposits to accumulate in the lenses of the eyes.
Experts believed that your chances of developing conditions like glaucoma and cataracts are about twice those of someone without diabetes.
What are the risk factors for diabetic eye disorders?
Anyone with diabetes can get diabetic eye disease. However, the risk increases if you have high blood glucose that is left untreated and high blood pressure that is not treated. High cholesterol levels and smoking can also increase the risk of diabetic eye disease. Certain groups of people are affected more than others. These include older adults who are at greater risk of losing vision or going blind due to diabetes mellitus.
Warning signs to watch for
In general, there are no early symptoms of diabetic eye disease. If you develop diabetes and eye issues, you may have no pain, no change in your vision, as damage to the eye is a gradual process, particularly with diabetic retinopathy. When symptoms develop, they appear as:
Blurry or wavy vision
Dark areas of vision loss
Flashes of light
Frequently changing vision
Poor colour vision
Cotton wool spots or dark stains
If you develop any of the above diabetes and the eyes symptoms, talk to your healthcare professional.
When to see an ophthalmologist?
Call your healthcare professional immediately if you experience sudden changes in your vision, including flashes of light or many spots, compared to your normal vision. You should see the healthcare specialist straight away if it feels like a curtain is pulled over your eyes. Such changes in your sight could be an indication of detached retina, which is considered a medical emergency. To prevent such side effects, incorporating diabetes and eye care management into your routine is crucial.
Takeaway!
Diabetes and eye care are closely linked. The best way to prevent diabetes and eye damage is to manage your blood sugar levels, as well as your blood pressure and cholesterol levels. Moreover, if you have been diagnosed with diabetes, be sure to have regular eye exams to assess your eye health and detect any changes.